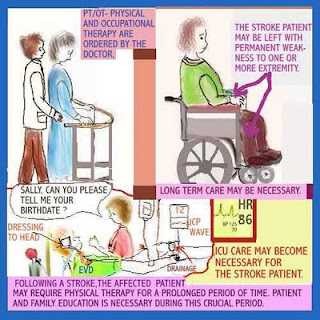
Generally there are three treatment stages for stroke: prevention, therapy immediately after the stroke, and post-stroke rehabilitation. To prevent a first or recurrent stroke (about 25 per cent of people who recovered from their first stroke will have another one within 5 years), the treatment is to identify and eradicate the risk factors, mentioned above. Acute stroke therapies try to stop a stroke while it is happening. In post-stroke rehabilitation physical therapy is essential, helping individuals to overcome disabilities that result from stroke damage. For the success of rehabilitating a stroke patient, the physical therapist should be able to reach all of these goals:, reduce muscles spasms, pain and stiffness, increase strength and function of affected arm and leg, roll/move in bed/sit/stand, retrain normal patterns of movement, increase energy levels, improvement of the balance and walking, reduce the risk of falls and increase independence and quality of life. [1]
In the initial phase of the stroke, while the patient is still in bed, physical therapist should move passively the arms and legs of the patient, always trying to ask the patient cooperation.
After the initial phase, the primary objective of the physical therapist is to help the patients to learn how to walk again. For that, the physical therapist will start firstly to increase the range of motion, the muscle tone, reduce the spasticity, improve his strength and to treat any shoulder pain, that is very common in stroke patients, like glenohumeral subluxation, development of adhesive capsulitis, neuritis of the nervus suprascapularis, bursitis subdeltoidea, tendovaginitis of the biceps tendons, neuropathy of the plexus brachialis, arthritis, thalamic pain, development of spasticity, Shoulder Hand Syndrome (SHS) or Sympathetic Reflex Dystrophy (SRD) [2].
Then will teach the patient how to move in bed, to prevent the formation of pressure ulceration. Once the patient is able to turn over in bed, the next step is to teach the patient to sit up unsupported in the bed. For this goal, the physical therapist will need to strengthen the trunk muscles in the seated position, promote the movement of the pelvis (anterior and posterior bascules), and the dissociation of waists, and the patients balance. Balance is often related to the terms stability and postural control. According to Pollock et al, sitting balance can be defined as “achieving, maintaining or restoring stability during a seated position or activity”. In rehabilitation, a satisfactory sitting balance is considered an important prerequisite for functional daily activities, such as getting dressed, reaching and eating. Remedying the asymmetric distribution of the body weight while sitting is regarded as an important part of the treatment of patients with stroke. Doing reaching exercises while the physical therapist tries to assure the stability of the trunk could be a good way to improve the patient’s stability. Some instruments to measure the sitting balance are the Trunk Control Test and the Time Balance Test [2].
After this, the physical therapist will teach the patient how to transfer from the bed to the wheelchair and vice-versa, and from the wheelchair to toilet and vice-versa. Being able to rise from a chair by oneself is an essential part of ADL activities, such as getting dressed, going to the toilet and walking. Some aspects that might influence standing up can be divided into factors that can be related to the chair (e.g. height of the seat), the patient (e.g. muscle strength in the legs), or strategy (e.g. speed, placing of the feet or attention). Some activities that the physical therapist can perform to evaluate the progression are: being to sit without support for 1 minute to 20 minutes, being able to stand up from a chair independently, being able to walk independently with or without walking aid, being able to walk a maximum of 10 steps. Exercising the standing up and sitting down results in an improvement of: the symmetry of balance during standing up and sitting down, the severity of the paresis, the speed of standing up and sitting down, walking speed, physical endurance and frequency of falls. It is recommended to do exercises of standing up and sitting down 30 minutes per day during several weeks to improve the left-right distribution of the body weight during these position changes [2].
After this goal is completed and well secure, the physical therapist usually will have the patient try to start walking, on the bars, then with assistive material (quadruped cane, two crutches, one crutch and a cane). Firstly, the patient should walk on a regular surface, then on an irregular surface (e.g. matress). To reach this goal there needs to be muscle strength, namely from the anti-gravity muscles, muscle endurance, and balance. Strength training is defined as the isometric or isokinetic strengthening of muscles by means of static or repetitive eccentric and/or concentric resistance exercises. Endurance training is defined as a training form with the primary goal of improving physical endurance, which is usually performed on a treadmill, rowing or cycle ergometer, often combined with exercises to improve ADL, focusing on repetitive exercises, such as standing up, sitting down, training on exercise steps and/or climbing stairs. Muscle strengthening has been found to have a positive effect on the strength of the paretic leg and on comfortable walking speed, and no negative effects were found in terms of increased spasticity, decreasing the muscle tone. Endurance training seems to show a positive trend towards improvement of physical endurance. Current knowledge suggests that a combination of strength and endurance training, using workstation (aerobics/fitness) offers added value for walking ability in all phases. It is recommended to train a minimum frequency of 2 to 3 times a week for a minimum of 30 minutes, with the help of fitness equipment or functional exercises, such as climbing stairs and walking over long distances on different surfaces. The balance can be improved by exercising stance control with visual feedback while standing on a force platform [2].
There some techniques that can be used by the physical therapist to improve the patient motor impairment caused by the stroke [1]:
Neurodevelopment treatment (Bobath)
Neurodevelopment treatment aims at inhibiting spasticity and synergies using inhibitory postures and movements and to facilitate normal autonomic responses that are involved in voluntary movement, which includes the gradual withdrawal of the direct input of the practitioner leading to increased independence.
Alexander technique
The Alexander technique works to change movement habits in our everyday activities. Improves the freedom of movement balance support and coordination. Teaches the use of the appropriate amount of effort for a particular activity giving you more energy for all your activities.
Rolfing
Rolfing consists on the manipulation of the soft tissues or myofacial system to allow for proper alignment and organization of the whole body in gravity. It helps loosen up spastic muscles and smoothes out gait patterns and helps keep the spine alignment.
Vojta Therapy (reflex locomotion)
The Vojta therapy is a highly specialized type of physical therapy that is designed to primarily enhance the motor development of a child. The treatment has added benefits of improvements in cognition fine motor breathing and digestion.
Muscle Re-education Approach
The ultimate goal of this approach is the development of co-ordinated movement patterns training begin with learning the control of individual muscles on a cognitive level.
Knott and Voss PNF Approach
PNF relies on quick stretch and manual resistance of muscle activation of the limbs in functional directions which are often spiral or diagonal.
Roods Sensorimotor Approach
The Roods Sensorimotor Approach involves superficial cutaneous stimulation using stroking, brushing, icing, or muscle stimulation with vibration to evoke voluntary activation.
Conclusion
The final goal of physical therapy in rehabilitating stroke patients is to achieve the best level of function and independence. Muscle weakness and loss of co-ordination are the primary impairments that affect gait after stroke, but impaired cardio-respiratory fitness may secondarily affect gait performance but limiting walking endurance.
Good balance and gait performance are key issues and main goals on the rehabilitation of stroke patients. [3]
[1] Parthiban, G. Role of Physiotherapy in Stroke. Aayushman Pain & Rehabilitation Clinic
[2] Peppen RPS van, Kwakkel G, Harmeling-van der Wel BC, Kollen BJ, Hobbelen JSM, Buurke JH, et al (2004). KNGF Clinical Practice Guideline for physical therapy in patients with stroke. Review of the evidence. Supplement to the Dutch Journal of Physical Therapy (Nederlands Tijdschrift voor Fysiotherapie): 114(5).
[3] Amatya, D.L. Post-stroke Physical rehabilitation. Nepal
Sem comentários:
Enviar um comentário